Re-engineering a TB Drug to Eliminate Dormant Persister Bacteria
Research Summary: We chemically modified moxifloxacin into a smart, enzyme-activated prodrug that easily enters bacteria and selectively kills dormant TB persisters, offering a blueprint to shorten therapy and reduce relapse.
Author interview

T. Anand Kumar earned his PhD from IISER Pune and is currently a postdoctoral researcher at Johns Hopkins University, USA. His research focuses on developing targeted radiotheranostics for cancer diagnosis and treatment.
Linkedin: https://www.linkedin.com/in/anandkt/
Twitter: @Anand_Kumar_T
Lab: Prof. Harinath Chakrapani, Indian Institute of Science Education and Research, Pune (IISER-Pune)
Lab website: https://www.hclab.in
What was the core problem you aimed to solve with this research?
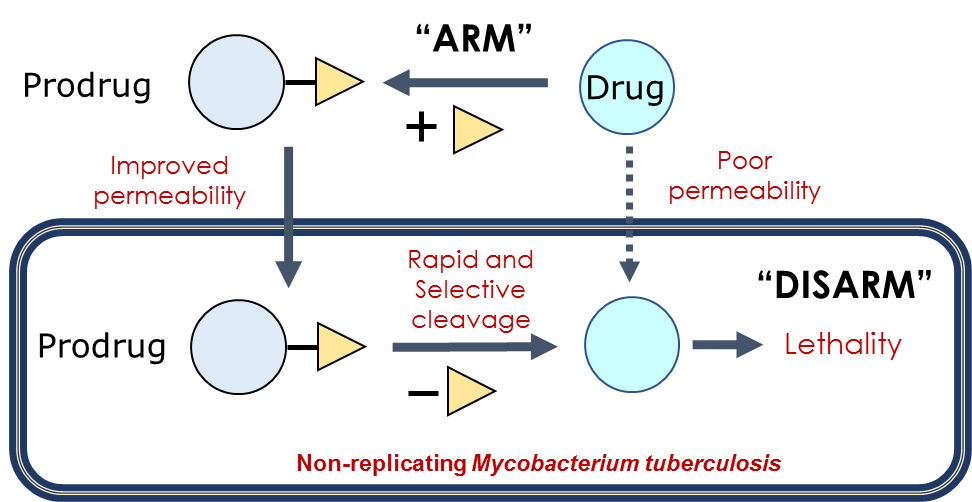
A major challenge in tuberculosis (TB) treatment is a small population of dormant “persister” bacteria that survive antibiotics, prolong therapy, and cause relapse. These non-replicating cells have poor drug permeability and enhanced drug efflux, leading to low intracellular drug accumulation and phenotypic antimicrobial resistance. Although moxifloxacin, a fluoroquinolone antibiotic has helped shorten TB therapy, non-replicating mycobacteria remain highly refractory to this and other frontline drugs, highlighting a critical unmet challenge in TB treatment.
How did you go about solving this problem?
We adopted an “arm-to-disarm” strategy by masking moxifloxacin as a prodrug to improve its permeability into TB bacteria. Once inside the bacteria, the prodrug is selectively activated by the enzyme nitroreductase (NTR) to release the active drug. This Trojan horse approach effectively reduces dormant persister populations, while retaining activity against actively growing replicating Mycobacterium tuberculosis (Mtb). Using a combination of chemistry, enzymatic studies, microbiological assays, and computational modeling, we identified a lead prodrug that not only outperforms moxifloxacin against persisters but also retained lethality against replicating bacilli.
How would you explain your research outcomes (Key findings) to the non-scientific community?
We found a way to make an existing frontline anti-TB drug antibiotic work better against the most stubborn TB bacteria. These bacteria can “hide” in a dormant state where most antibiotics fail. We chemically modified the drug into a temporarily inactive form, called a prodrug, that can easily enter the bacteria and become active once inside, allowing the bacteria’s own machinery to release a drug that kills them. This approach made the drug much more effective at eliminating these hard-to-kill cells, which are responsible for long treatment times and disease relapse.
This study demonstrates that re-engineering existing drugs into enzyme-activated prodrugs can overcome phenotypic antimicrobial tolerance in non-replicating TB bacteria. — Prof. Harinath Chakrapani
What are the potential implications of your findings for the field and society?
Our findings offer a practical way to improve tuberculosis treatment by enhancing the effectiveness of existing, widely used TB drugs against hard-to-kill persister bacteria. This prodrug-based “arm-to-disarm” strategy could help shorten treatment duration, reduce relapse, and slow the emergence of drug resistance. By repurposing well-tolerated antibiotics rather than developing entirely new drugs, this approach may accelerate the translation of improved therapies, with significant benefits for global TB control and public health.
What was the exciting moment during your research?
One of the most exciting moments was identifying a lead prodrug that was rapidly and efficiently converted into the active drug under all experimental conditions and showed strong correlation with bacterial killing. Additionally, developing a mathematical model that linked drug permeability, prodrug activation, and bacterial killing helped us clearly rationalize why higher intracellular drug levels are required to eliminate non-replicating TB bacteria.
Paper reference/citation (with link): Kumar, T. A., Birua, S., Mallojjala, S. C., Mukherjee, P., Singh, S., Kaul, G., Ramachandran, A., Akhir, A., Chopra, S., Gadgil, C. J., Hirschi, J. S., Singh, A., & Chakrapani, H. (2025). A Mycobacteria-Specific Prodrug to Overcome Phenotypic AMR in Mycobacterium tuberculosis. J. Med. Chem. 2025, 68 (23), 24935–24952. doi: https://doi.org/10.1021/acs.jmedchem.5c01848
Explore more
🎤 Career – Real career stories and job profiles of life science professionals. Discover current opportunities for students and researchers.
💼 Jobs – The latest job openings and internship alerts across academia and industry.
🛠️ Services – Regulatory support, patent filing assistance, and career consulting services.




