Kerala is grappling with a surge in deaths caused by a rare but often fatal brain infection known as Primary Amebic Meningoencephalitis (PAM), usually due to Naegleria fowleri—the so-called “brain-eating amoeba.” As of late August / early September 2025, at least six people have died in Kerala, with several more cases under treatment. Victims include children and adults.
What Is Naegleria fowleri and How It Enters the Brain
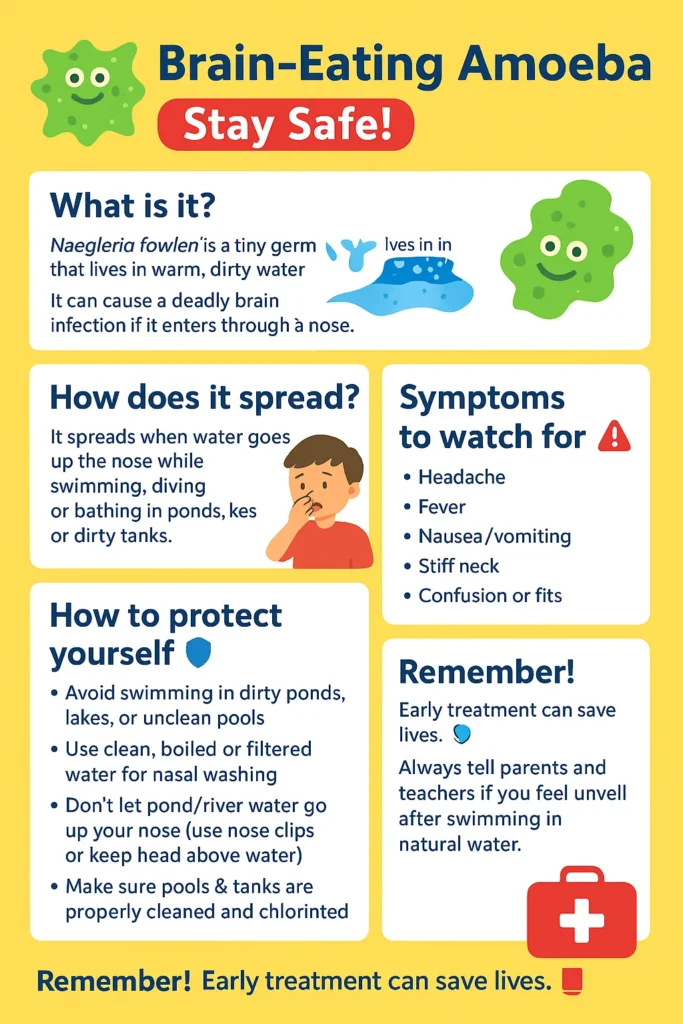
- Naegleria fowleri is a free-living amoeba found in warm freshwater bodies—ponds, lakes, rivers, and poorly chlorinated pools especially when the water temperature is high. (CDC)
- It does not infect by drinking water. Instead, infection happens when contaminated water enters the nose (for example, while swimming, diving, or bathing). From the nose, the amoeba travels along the olfactory nerve to the brain, where it begins damaging brain tissue. PAM is characterized by rapid onset and severe inflammation and destruction of brain tissue. (CDC)
Symptoms: What to Watch For
In the initial days after exposure, symptoms are often vague and may mimic viral or bacterial meningitis:
- Fever
- Severe headache
- Nausea, vomiting
- Sometimes stiff neck
These are followed by more serious signs as the infection worsens:
- Confusion or altered mental state
- Seizures
- Loss of balance
- Coma (Cleveland Clinic)
Because the disease progresses fast, often within days, early recognition is crucial. (NCBI)
History: When Was Naegleria fowleri First Discovered?
- The pathogen Naegleria fowleri was identified and studied in the mid-20th century among free-living amoebae.
- Cases of human infection have always been rare but nearly always very serious. Before recent years, survival was extremely uncommon. (Gavi)
Treatments: What Medicines Are Available
There is no guaranteed cure, but certain medicines and treatment combinations have shown success when used very early:
- Amphotericin B is considered the primary antifungal used against Naegleria infections. (CDC)
- Other drugs often used in combination include miltefosine, azoles (such as fluconazole or posaconazole), azithromycin, rifampin, and steroids (to reduce brain inflammation). (CDC)
- Because confirmed survivors are very few globally, treatment is experimental, urgent, and generally aggressive. (CDC)
Why It’s Vital to See a Doctor Early
- PAM progresses very rapidly—from symptom onset to severe brain damage or death can be just several days. Delayed diagnosis sharply reduces chances of survival. (NCBI)
- Early treatment increases the odds of survival; when cases are caught late, the infection often is already advanced. (CDC)
- Also, symptoms of PAM are similar to those of more common conditions (e.g. viral or bacterial meningitis). A healthcare professional needs to be aware of PAM, consider it in diagnosis especially if there has been freshwater exposure, order appropriate lab tests, and begin treatment immediately.
How to Protect Yourself: Precautionary Measures
Because infections are rare but deadly, prevention is the best strategy. Here’s what you can do:
- Avoid swimming or bathing in warm, stagnant, unclean freshwater bodies, especially ponds, lakes, or rivers during the hot season.
- Keep water out of your nose when in such waters—use nose clips or hold your nose shut. Let your head stay above water when possible. (CDC)
- Use only boiled, sterilized, or distilled water for any nasal cleaning, ablutions, or rituals that involve water entering the nose. Tap water can harbor the amoeba. (CDC)
- Ensure proper chlorination and good maintenance of public pools, wells, and water storage tanks. Clean and disinfect them regularly.
- Public awareness plays a big role—knowing the risk, recognizing symptoms, and seeking help early are key.
Important Context in Kerala
- The state has reported dozens of suspected or confirmed cases in 2025.
- Deaths include both children and adults.
- Authorities are stepping up preventive campaigns: chlorination of wells and ponds, posting warning signs at water bodies, education drives, surveillance of symptoms in health centers.
Bottom Line
While “brain-eating amoeba” cases are rare, their outcomes are almost always grave unless caught very early. Recognizing risk situations (warm stagnant water, nasal exposure), knowing the early symptoms, and consulting a doctor immediately can make the difference between life and death.
Protect your nose, your water, your awareness—and seek medical help fast if anything feels wrong after exposure.
Stay safe, stay informed. And if there are any updates in treatment or local alerts, check with trusted public health sources or your nearest healthcare provider.
Explore more
🎤 Career – Real career stories and job profiles of life science professionals. Discover current opportunities for students and researchers.
💼 Jobs – The latest job openings and internship alerts across academia and industry.
📢 Advertise with BioPatrika – Reach the Right Audience, Fast!
🛠️ Services – Regulatory support, patent filing assistance, and career consulting services.




