Polycystic Ovary Syndrome (PCOS) is often thought as just a reproductive disorder due to missed periods, acne, obesity and infertility. But this common condition that affects around 1 in 10 women globally, is much more than a mere hormonal hiccup. It is a complex metabolic and endocrine disorder that quietly increases the risk for serious long-term diseases, including certain cancers.
In my academic journey while studying about gynaecological cancers, I have noticed how PCOS is often sidelined as a cancer-risk. In this article, I explore how PCOS may contribute to cancer development, and why awareness and early intervention really matters.
What is PCOS?
PCOS is one of the most common yet underestimated endocrine disorders affecting individuals with ovaries. Clinically, it is characterized by irregular or absence of ovulation (reduced or lack of periods), excess androgen levels, and visible appearance of ovaries bearing multiple cysts (polycystic ovaries) via ultrasound. However, this clinical definition barely scratches the surface.
Despite its prevalence, PCOS is not a homogenous condition. It exists on a spectrum, often overlapping with obesity, insulin resistance, thyroid dysfunction, and mood or psychological disorders. Yet, many of its underlying molecular mechanisms remain poorly understood, making both diagnosis and treatment challenging.
Global and Indian Statistics
Globally, PCOS affects around 8–13% of women of reproductive age, but the numbers may significantly vary due to diagnostic ambiguity and sociocultural silence. In India, some studies suggest prevalence as high as 20–25% in urban populations, with a rising trend among adolescents.
What makes PCOS particularly insidious is that many affected individuals may not seek help until fertility becomes a concern, and by the time metabolic and hormonal dysregulation may have set in and festered for years.
The Biochemistry of PCOS: What Is Measurable and Diagnosable
Though PCOS is a clinically heterogeneous syndrome, it exhibits a set of measurable biochemical features that help guide diagnosis and management. These are not speculative mechanisms rather they are diagnostic or supportive laboratory findings that reflect the metabolic and endocrine disruptions underlying the condition.
Here’s what is commonly observed:
-
Elevated Androgens/male hormones (Hyperandrogenemia)
Most PCOS diagnoses involve raised levels of testosterone, androstenedione, or DHEAS. These androgens disrupt follicular development and contribute to clinical symptoms like acne, hirsutism, male pattern baldness in females and anovulation.
-
Altered Gonadotropin Ratios
Many PCOS patients show a raised LH:FSH ratio, often greater than 2:1. This imbalance promotes androgen production from the theca cells and interferes with normal follicular maturation.
-
Low Sex Hormone Binding Globulin (SHBG)
SHBG, produced in the liver, binds to androgens and oestrogens, reducing their bioavailability. Hyperinsulinemia, often present in PCOS, suppresses SHBG synthesis, increasing the levels of free (biologically active) testosterone in the blood.
-
Insulin Resistance (IR) and Hyperinsulinemia
Insulin resistance is observed in up to 70% of women with PCOS, including those who are lean. It can be measured by elevated fasting insulin levels, glucose-insulin ratios, or surrogate indices like HOMA-IR.
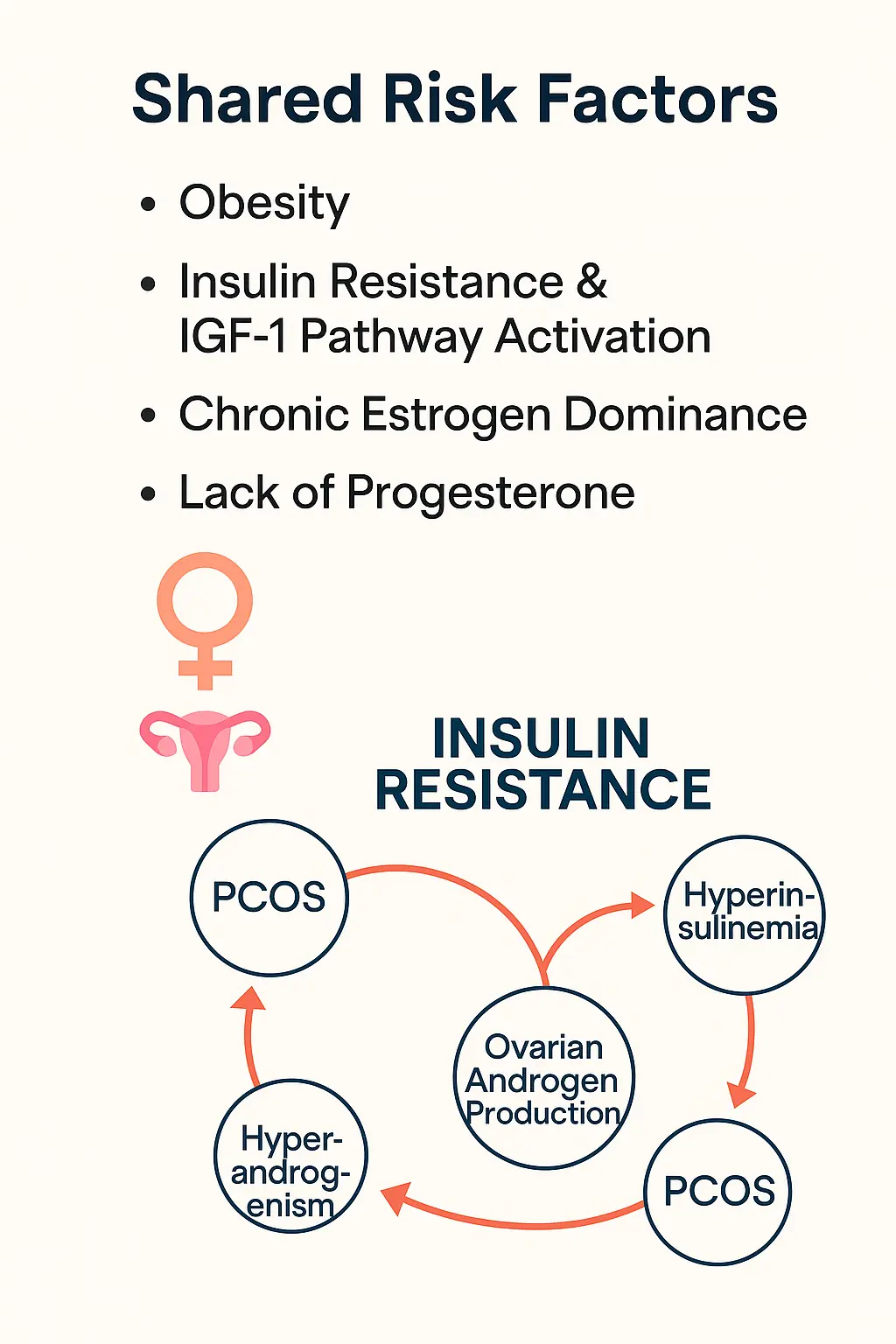
Though not a diagnostic criterion for PCOS, insulin resistance plays a central role as a biochemical amplifier in amplifying its endocrine and metabolic features. High insulin levels stimulate ovarian androgen production, reduce SHBG, and can disturb the hypothalamic-pituitary-gonadal axis, worsen ovulatory dysfunction, and increase the risk for metabolic syndrome and endometrial hyperplasia.
-
Elevated Fasting Glucose or Impaired Glucose Tolerance
Women with PCOS are at a significantly higher risk of developing pre-diabetes or type 2 diabetes, often diagnosed via fasting plasma glucose, oral glucose tolerance tests (OGTT), or HbA1c. These parameters are not just metabolic problems, they may also indicate future risks such as endometrial cancer, which has strong links to insulin and oestrogen signalling.
There is still no consensus on whether insulin resistance initiates the syndrome or arises because of androgen excess, chronic inflammation, or obesity. The reality may lie in both directions, depending on the phenotype of the individual.
PCOS and Cancer: What We Know So Far
Owing to the hormonal and metabolic mayhem characteristic of PCOS including obesity, insulin resistance, chronic oestrogen dominance, and progesterone deficiency, several studies have pointed to an increased risk of certain cancers, particularly when the condition is left unmanaged.
-
Endometrial Cancer (Cancer of the inner lining of the uterus)
The strongest and most consistent link. Chronic anovulation leads to prolonged unopposed oestrogen exposure without progesterone, causing endometrial hyperplasia which is a known precursor to cancer.
-
Ovarian Cancer
Data here is mixed. Some studies suggest a slight increase in risk, especially in women who undergo repeated ovulation-induction treatments. However, other studies show no significant correlation.
-
Breast Cancer
Findings are inconclusive. While some subtypes (e.g., hormone-receptor-positive breast cancers) may show a slight risk elevation, the direct correlation to PCOS remains elusive.
Lifestyle: The Double-Edged Sword
Modern lifestyles are amplifying PCOS risk. Sedentary behaviour, high glycaemic diets, chronic stress, and poor sleep patterns all exacerbate the hormonal and metabolic disturbances central to PCOS.
However, it is important not to fall into the trap of blaming lifestyle alone. While these factors influence severity and progression, they are not always the root cause. Many lean women with active lifestyles also develop PCOS, indicating that genetics, epigenetics, and environmental exposures are all contributing.
What Can Be Done? Steps Toward Prevention and Control
Although there’s no “cure,” PCOS can be managed effectively and by doing so, one can also reduce long-term cancer risks.
Medical Interventions (After consultation with the physicians):
- Cyclical Progesterone or Oral Contraceptives: Protect the endometrium and regulate cycles.
- Metformin: Improves insulin sensitivity.
- Anti-androgens: For hyperandrogenic symptoms like acne and hirsutism.
Lifestyle Strategies:
- Balanced Diet: Low in refined carbs and sugars; rich in fibre and healthy fats.
- Physical Activity: Even moderate exercise improves insulin sensitivity.
- Weight Management: Even a 5–10% weight loss can restore ovulation in many cases.
Regular Screening:
- Transvaginal ultrasounds, endometrial biopsies (when indicated), and hormonal panels should be used judiciously to monitor risk.
Final Thoughts
PCOS is not merely a cosmetic or fertility issue. It’s a metabolic and endocrine disorder with underestimated oncogenic potential. While the biochemistry remains partly elusive, the clinical patterns are becoming clearer that PCOS increases susceptibility to certain cancers through prolonged hormonal imbalance, chronic inflammation, and insulin resistance.
We need to move beyond the reductionist idea that PCOS is purely a “lifestyle disease.” By acknowledging its systemic nature and investing in deeper research especially in the Indian context, we can empower individuals with the knowledge and tools to take preventive action.
The connection between PCOS and cancer may be hiding in plain sight, but awareness can bring it into focus.
References
- Barry, J. A., Azizia, M. M., & Hardiman, P. J. (2014). Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: A systematic review and meta-analysis. Human Reproduction Update, 20(5), 748–758. https://doi.org/10.1093/humupd/dmu012
- Chittenden, B. G., Fullerton, G., Maheshwari, A., & Bhattacharya, S. (2009). Polycystic ovary syndrome and the risk of gynaecological cancer: a systematic review. Reproductive Biomedicine Online, 19(3), 398–405. https://doi.org/10.1016/S1472-6483(10)60003-7
- Shan, B., Cai, J., Li, M., Yu, Y., & Pan, X. (2020). Polycystic ovary syndrome and risk of endometrial, ovarian, and breast cancer: a meta-analysis. Endocrine-Related Cancer, 27(6), 295–308. https://doi.org/10.1530/ERC-19-0493
- Shetty, C., Rizvi, S. M. H. A., Sharaf, J., Williams, K. D., Tariq, M., Acharekar, M. V., Guerrero Saldivia, S. E., Unnikrishnan, S. N., Chavarria, Y. Y., Akindele, A. O., Jalkh, A. P. C., Eastmond, A. K., & Hamid, P. (2023). Risk of Gynecological Cancers in Women With Polycystic Ovary Syndrome and the Pathophysiology of Association. Cureus, 15(4), e37266. https://doi.org/10.7759/cureus.37266
- WHO. (2023). Polycystic Ovary Syndrome Fact Sheet. https://www.who.int/news-room/fact-sheets/detail/polcystic-ovary-syndrome
- Wu, D., Zhang, Y., Wu, C., An, B., Wang, X., Ni, J., & Chen, M. (2025). The relationship between polycystic ovary syndrome and gynecological cancers: Neurotransmitter metabolism changes and immune regulation. Frontiers in Immunology, 16, Article 1578470.
About the Author
Bhadra Pattanayak is a researcher with a background in cancer biology and biochemistry, currently exploring intersections between endocrine health and oncology.
Disclaimer: The author used ChatGPT (GPT-4, OpenAI, July 2025) to assist with structuring and editing parts of the article. All scientific content was reviewed and verified by the author.
Explore more
🎤 Career – Real career stories and job profiles of life science professionals. Discover current opportunities for students and researchers.
💼 Jobs – The latest job openings and internship alerts across academia and industry.
📢 Advertise with BioPatrika – Reach the Right Audience, Fast!




