Cancer continues to be one of the biggest health challenges in the world. Traditional treatments like surgery, chemotherapy and radiation have saved many lives, but they often come with strong side effects, and cancer can sometimes return even after treatment. Over the last decade, a new approach called immunotherapy has brought hope to patients by helping the body’s own immune system to fight cancer.
One of the most successful immunotherapy strategies is called the immune checkpoint blockade. Normally, immune cells work like soldiers protecting the body. But cancer cells are clever — they put on a “disguise” to hide from these soldiers. A major disguise molecule they use is called PD-L1. When PD-L1 on cancer cells attaches to a partner protein PD-1 on immune cells, it sends a message like “Don’t attack me.” Because of this, T-cells — which normally kill harmful cells — become inactive.
To overcome this, scientists developed medicines that block PD-L1 or PD-1, removing the disguise so the immune system can recognize and destroy cancer cells. These drugs have helped patients with lung, skin, bladder and several other cancers — a milestone recognized by the 2018 Nobel Prize in Medicine.
The Challenge: Not Everyone Benefits
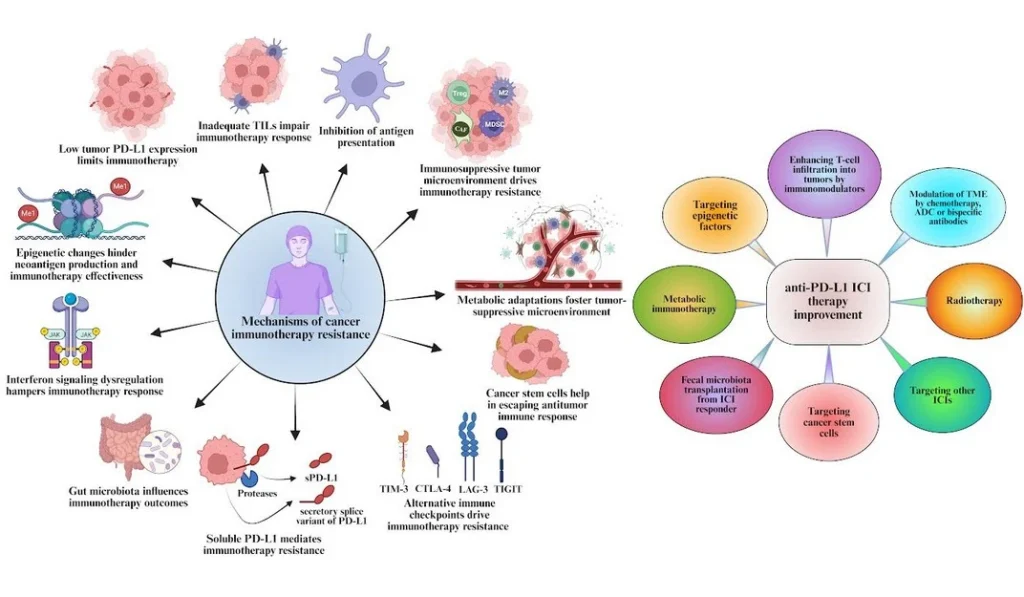
Even though anti-PD-1/PD-L1 immunotherapy has changed cancer treatment, it does not work for most patients. Only about 15–25% of patients respond well. Some do not respond from the very beginning (primary resistance), while others respond initially but later the cancer returns (acquired resistance).
Why does this happen? In this review article, the authors (Kartik Mandal, Ganesh Kumar Barik, PhD, and Manas Santra) explain several reasons:
- Some tumors have very little PD-L1, so these drugs have nothing to block
- Some tumors don’t allow immune cells to enter — called “cold” tumors
- Cancer cells may hide their antigens, so T-cells cannot find them
- The tumor can change the environment around it to suppress immunity
- Tumors may activate other immune-blocking pathways
- Genetic and hormonal differences can make men and women respond differently
Because of these complexities, choosing which patient will benefit from immunotherapy is still difficult.
Making Immunotherapy More Effective
This review highlights several new strategies that researchers are exploring:
🔹 Combination treatments – immunotherapy with chemotherapy, radiation, targeted therapy, CAR-T cell therapy, or metabolic drugs
🔹 Changing the tumor microenvironment to allow more immune cells to attack
🔹 Neoantigen-based personalized therapies – teaching the immune system to target unique cancer markers
🔹 New biomarkers like tumor mutational burden (TMB) and circulating PD-L1 in blood
🔹 Artificial intelligence and multi-omics technology to better predict who will respond
🔹 Liquid biopsy for real-time monitoring of treatment progress
These innovative approaches aim to convert more “cold” tumors into “hot” ones and help more patients benefit from immunotherapy.
Looking Ahead
The future of cancer treatment lies in precision immunotherapy — giving the right treatment to the right patient at the right time. This review emphasizes the need to:
✔ Understand how cancer escapes the immune system
✔ Identify smarter biomarkers to select suitable patients
✔ Design personalized and combination therapies
✔ Continue clinical trials with advanced technologies
Immunotherapy has already improved the lives of many cancer patients, but with deeper scientific understanding and collaboration, we can expand that success to many more.
Reference: Overcoming resistance to anti-PD-L1 immunotherapy: mechanisms, combination strategies, and future directions. 🔗 https://doi.org/10.1186/s12943-025-02400-z
—
Kartik Mandal
Explore more
🎤 Career – Real career stories and job profiles of life science professionals. Discover current opportunities for students and researchers.
💼 Jobs – The latest job openings and internship alerts across academia and industry.
🛠️ Services – Regulatory support, patent filing assistance, and career consulting services.




